3. Telomere length predicts lifespan
For a long time we thought that our cells might be immortal, and that under the right environmental conditions, they would go on replicating forever. But, as discovered in 1961, they don’t: after some 50 to 70 divisions, they stop. A decade later a hypothesis was put forward: telomeres – repeated DNA sequences at the ends of our chromosomes – shorten with every division, and when they get too short, divisions stop and the cells die.
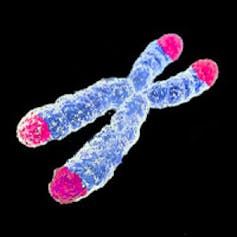
Since then, there has been increasing evidence that telomere length can be used to predict lifespan, and not just in humans. However, not all researchconfirms this, and it is not yet clear whether shortened telomeres are the cause of ageing or just a symptom. If telomere length does control ageing, then it may be possible to significantly lengthen lifespans by manipulating their length. At the moment we still know too little about telomeres to do this, but watch this space.


